The Urinary Bladder and Urinary Incontinence
by Robert Tallitsch, PhD | June 23, 2025
Case study video explaining the urinary bladder and urinary incontinence with a patient example!
Use the button below to schedule a demo to learn about our quizzes, flash cards, and other anatomy resources that support this Brain Builder!
Schedule a Demo
Bladder control problems are quite common. However, the inability to control your bladder can be either a small annoyance or a major problem that affects one’s quality of life — depending on the degree of incontinence. According to the Urology Care Foundation, millions of adults in the United States experience urinary incontinence. Statistically, twice as many women develop urinary incontinence as men.
In this Brain Builder, we will discuss the anatomy of the urinary bladder, its sphincters, and the neurological control of these structures. Then, we will discuss the various types of urinary incontinence, symptoms, causes, and treatments.
The Urinary Bladder
The urinary bladder is a smooth muscular sac shaped like an inverted pear. The bladder, which serves as a reservoir for the urinary system, holds approximately 300 to 500 cubic centimeters of urine when full.
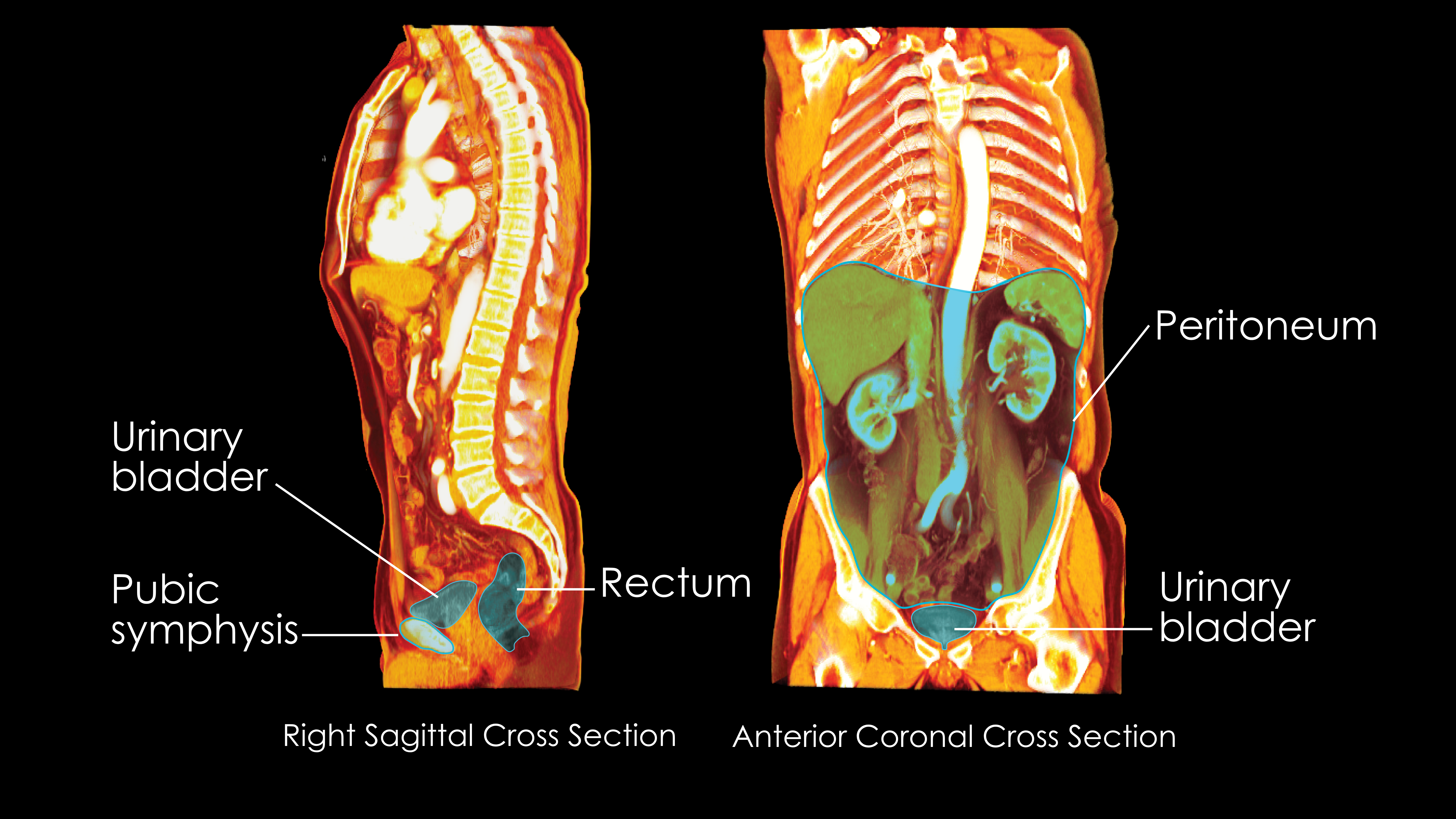
The position of the urinary bladder is dependent upon the fullness of the bladder. However, the urinary bladder is described as lying:
- inferior to the peritoneum and being covered by coils of the small intestine
- posterior to the pubic symphysis
- anterior to the rectum and the termination of the vas deferens and the seminal vesicles in males and anterior to the vagina and the superior vaginal part of the cervix in females
- medial to the levator ani and the obturator internus muscle
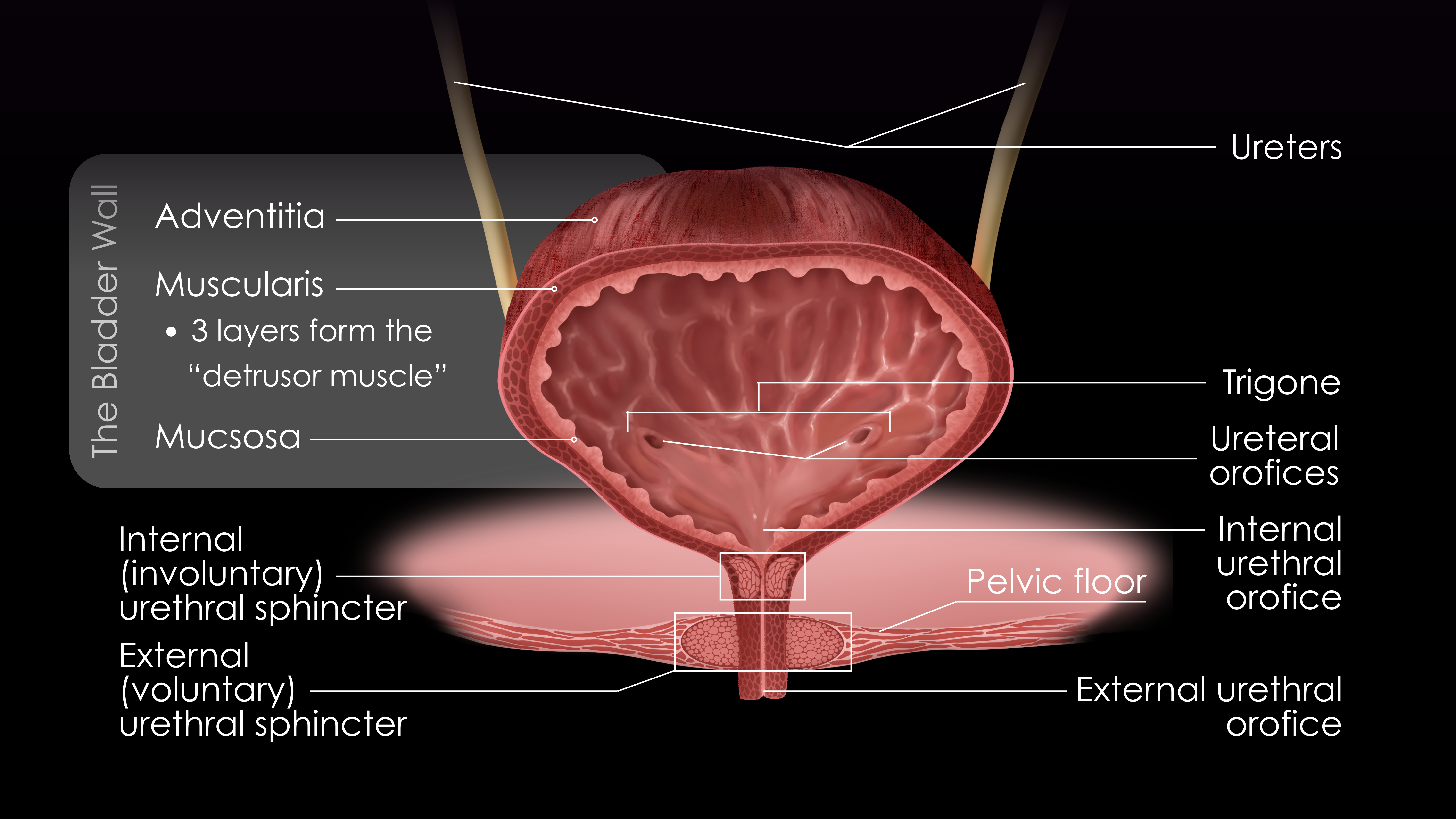
The wall of the urinary bladder is composed of the mucosa, muscularis, and adventitia. The muscularis has three layers of intertwining smooth muscle. These muscular layers are sometimes collectively referred to as the detrusor muscle.
At the inferior aspect of the bladder is the trigone, a triangular structure composed of the superior, lateral ureteral orifices (openings of the ureters into the bladder) and the inferiorly and centrally located internal urethral orifice. Surrounding the internal urethral orifice is the involuntary urinary sphincter of the urinary bladder. Because of the arrangement of the detrusor muscle fibers, the involuntary urinary sphincter is closed when the detrusor muscle is relaxed. Contraction of the detrusor muscle changes the shape of the involuntary sphincter, causing it to open.
Just inferior to the involuntary urinary sphincter the urethra is surrounded by a ring of voluntary skeletal muscle, which forms the voluntary urethral sphincter.
Vascular Supply of the Bladder
The superior and inferior vesicle branches of the internal iliac arteries supply blood to the bladder. The vesicle branches of the bladder form a venous plexus that drains into the inferior iliac vein.
Innervation of the Bladder
The urinary bladder is innervated by both the sympathetic and parasympathetic branches of the autonomic nervous system. Sympathetic fibers originate from the L1 and L2 segments of the spinal cord. Parasympathetic fibers originate from the S2, S3, and S4 segments of the spinal cord.
Micturition
When the bladder is empty, there is little activity of the parasympathetic nervous system upon the detrusor muscle fibers. However, there is considerable sympathetic activity upon the involuntary urinary sphincter at this time, causing the sphincter to remain closed.
Two neurological processes control the emptying of the urinary bladder.
- Spinal Cord Reflex:
a. As the urinary bladder fills, stretch receptors within the wall of the urinary bladder become activated. Afferent nerves from these stretch receptors cause activation of the parasympathetic fibers within the spinal cord. This parasympathetic nervous system activation causes the detrusor fibers to contract. This contraction also changes the shape of the internal sphincter, causing it to open.
b. The afferent nerves from the stretch receptors within the urinary bladder also inhibit the sympathetic nervous fibers within the spinal cord. This decreases sympathetic nervous system activity, facilitating the opening of the internal sphincter.
2. CNS Stimulation:
Descending fibers from the brain have the ability to affect this reflexive emptying of the urinary bladder. This enables one to voluntarily initiate urination or prevent involuntary urination.
Urinary Incontinence
As one ages the muscles supporting the bladder tend to weaken, which may lead to incontinence. A variety of pathologies, ranging from cancer, kidney stones, an enlarged prostate, or bladder infection can initiate urinary incontinence. Urinary incontinence may be a temporary condition, such as that caused by a urinary tract infection, or it may be a permanent issue, such as neurological incontinence.
Urinary incontinence is described as the inability of an individual to control the emptying of their bladder. Current medical literature describes six types of urinary incontinence:
- Reflex (neurological) incontinence: Here the bladder muscle contracts without any warning or urge, causing a large urine leak. This typically occurs following damage to the sensory nerves that provide information about the filling of the bladder. This type of incontinence is found in individuals with spinal cord injuries or in individuals with multiple sclerosis.
- Overflow incontinence: This occurs in individuals who are unable to completely empty their bladder, either due to prostate enlargement, tumors, scar tissue, urinary bladder stones, or an underactive bladder (which eliminates the feeling of the need to urinate). Eventually, the bladder becomes overfilled, which changes the shape of the internal sphincter, causing it to change shape and allowing urinary leakage.
- Functional incontinence: Here the urinary tract is functioning properly, but the individual has one or more other underlying pathologies that prevent the bladder from emptying properly. Some of these complications include kidney damage, mental health side effects, cellulitis, and urinary tract infections.
- Stress incontinence: With stress incontinence increased abdominal pressure puts pressure on the bladder, causing spontaneous emptying. In this type of incontinence, the pelvic floor muscles or the urethral sphincter have become weakened. The word “stress” in this medical condition refers to the physical strain associated with the bladder leakage (rather than mental stress). This strain can be caused by laughing, jumping, or coughing.
- Urge incontinence (also termed overactive bladder): With this type of incontinence, an individual will feel an extreme urge to urinate, even though the bladder is not full. The extreme urge to urinate causes bladder leakage before the individual is able to reach the bathroom.
- Mixed incontinence: Here the individual has symptoms of both an overactive bladder and stress incontinence.
Treatment
Following a diagnosis of incontinence a physician may suggest one or more of the following treatment options, depending on the degree of incontinence and the perceived duration of the problem:
- Bladder training: This involves certain exercises to strengthen the muscles of the pelvic floor.
- Condition management: If one’s urinary incontinence is caused by a different underlying condition (such as a urinary tract infection) treatment of that condition may help reduce or eliminate the urinary incontinence.
- Behavior therapy: This might include one or more of the following changes in the individual’s lifestyle;
- Using the bathroom prior to the urge to urinate
- Weight loss: The loss of weight may reduce pressure on the bladder, which may reduce or eliminate incontinence.
- Use of a catheter: The usage of a urinary catheter may be recommended if the incontinence becomes severe.
- Use of absorbent undergarments
Although urinary incontinence may be minor, the effect on one’s quality of life typically causes an individual to seek medical advice. With the proper treatment urinary incontinence may be controlled or treated and, therefore, the effect on one’s quality of life may be minimized.
Key Terms
Urinary incontinence - The inability of one to control the emptying of their bladder.
Detrusor muscle - Another name utilized to describe the muscular layers of the urinary bladder.
Trigone - A triangular structure composed of the superior, lateral ureteral orifices (openings of the ureters into the bladder) and the inferiorly and centrally located internal urethral orifice found at the inferior aspect of the bladder.
Micturition - The process by which the bladder empties.
Arterial vessels supplying blood to the urinary bladder - The superior and inferior vesicle branches of the internal iliac arteries.
Bladder training - Certain exercises to strengthen the muscles of the pelvic floor and thereby reduce urinary incontinence.
Urge incontinence - A type of incontinence in an individual will feel an extreme urge to urinate, even though the bladder is not full. The extreme urge to urinate causes bladder leakage before the individual is able to reach the bathroom.
Overflow incontinence - A type of incontinence that occurs in individuals who are unable to completely empty their bladder, either due to prostate enlargement, tumors, scar tissue, urinary bladder stones, or an underactive bladder (which eliminates the feeling of the need to urinate). Eventually, the bladder becomes overfilled, which changes the shape of the internal sphincter and allows urinary leakage.
Schedule a demo today to learn how you can incorporate BodyViz into your classes and give your students the opportunity to practice using the information from this Brain Builder on real patients with authentic 3D dissection!
Schedule a Demo
Helpful Links: