The Integumentary System and Melanoma
by Robert Tallitsch, PhD | September 20, 2023
.jpg)
Video explaining the layers of the integument and a melanoma patient case example!
Use the button below to schedule a demo to learn about our activities, flash cards, and other anatomy resources that support this Brain Builder.
Schedule a Demo
The integumentary system, or integument, is composed of the skin and its derivatives (nails, hair, and glands). The functions of the integument include
- Protection
- Synthesis and storage of lipids
- Excretion of wastes
- Regulation of body temperature
- Synthesis of vitamin D3
- Coordination of immune responses involving cancers and other pathogens of the skin
- Sensing environmental stimuli
Even though the skin is one of, if not the largest organ of the body, a description is often omitted from human anatomy texts, and skin is seldom studied in the dissection laboratory. This Brain Builder will describe the anatomy of the skin and melanoma — the most dangerous form of skin cancer.
The Epidermis
The skin, or integument, is composed of two layers: a superficial epidermis, and a deeper dermis. The epidermis is composed of a keratinized stratified squamous epithelium. There are two types of skin: thick and thin. Thick skin, which typically lacks hair, is found on the palms of the hands and soles of the feet, and has fives layers. These layers are, from deep to superficial, the stratum basale, stratum spinosum, stratum granulosum, stratum lucidum, and stratum corneum.
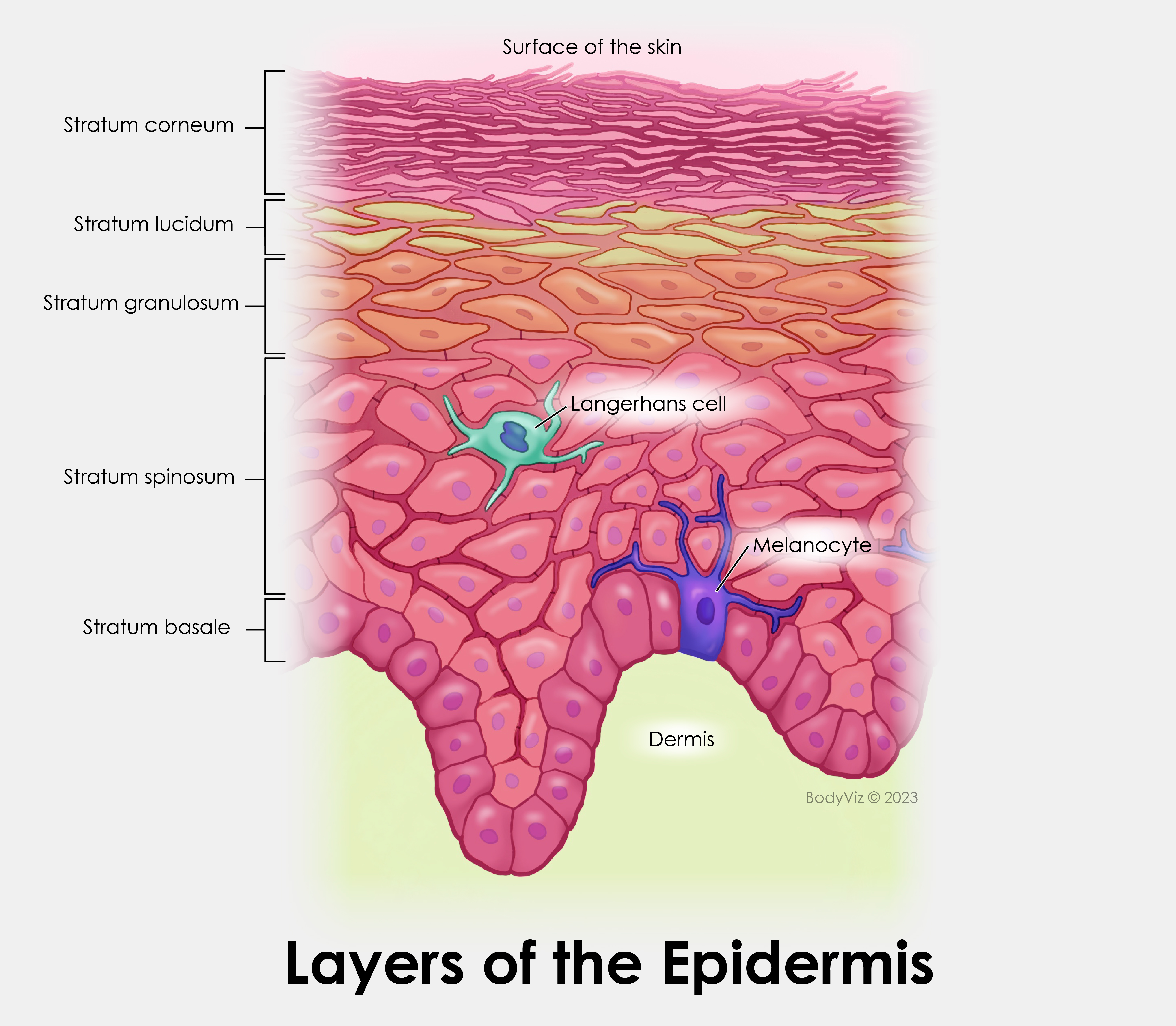
The deepest layer of thick skin is the stratum basale (also termed the stratum germinativum). This layer, which is one cell thick, is the epidermal layer with the highest rate of mitotic activity. As new cells are formed, they move superficially. This upward migration of new cells allows for the replacement of cells that are sloughed off and lost from more superficial layers of the epidermis.
Scattered within the stratum basale are pigment-producing cells called melanocytes. These cells possess cytoplasmic processes that inject pigment into adjacent cells within the stratum basale, as well as cells of more superficial layers. The pigment produced by melanocytes varies in color, from black to brown or yellow-brown. Differences in skin color are due to the rate of pigment synthesis, rather than the number of melanocytes present.
The next layer is the stratum spinosum. New cells produced by mitosis within the stratum basale migrate superficially into the stratum spinosum, which is several cell layers thick. Cells within the deepest part of the stratum spinosum continue to undergo mitosis, contributing to the thickness of this layer. Cells within this layer are characterized by possessing intracellular and intercellular specializations that tightly tie all of the cells within this layer together.
Melanocytes and Langerhans cells (also termed dendritic cells) are frequently found within this layer. Langerhans cells contribute to the immune response of the skin against skin cancers and pathogens that have penetrated the skin.
Superficial to the stratum spinosum is the stratum granulosum. Cells within this layer have moved superficially out of the stratum spinosum. This is the last layer of the skin where all of the cells possess a visible and functioning nucleus. Cells of the stratum granulosum synthesize large amounts of two intracellular proteins: keratin and keratohyalin. These proteins, once fully formed, will assist in protecting the skin from environmental microorganisms.
Stratum granulosum cells release granules by exocytosis. These granules contain a lipid-rich substance that will, in more superficial layers, completely coat all of the cells and contribute to the cells’ water resistance.
The stratum lucidum, which is superficial to the stratum spinosum, is found only within thick skin. Cells within this layer lack organelles and a functioning nucleus, and are densely packed together. The keratin proteins are fully formed and bind the cells of this layer tightly together.
The most superficial layer is the stratum corneum. This layer is composed of dead cells that possess a very thick cellular membrane, lack any organelles or nucleus, and possess a high amount of keratin. The intercellular connections formed within the stratum spinosum are still fully intact and bind the cells tightly together. In addition, the lipid-rich substance formed by the cells of the stratum granulosum completely surrounds the cells of this layer. These characteristics contribute to the protective nature of the stratum corneum against environmental pathogens and contribute to the cells’ water resistance.
The Dermis
Deep to the epidermis is the dermis, which is composed of two layers: a reticular layer and a papillary layer.
The reticular layer is the deepest layer of the dermis. This layer is composed of densely interwoven connective tissue fibers that surround blood vessels, nerves, hair follicles, sweat glands, and sebaceous glands. The connective tissue fibers of this layer extend deeper into the subcutaneous tissue, and superficially into the papillary layer. As a result, all of these layers are held tightly together.
The papillary layer of the dermis, which serves to mechanically anchor the epidermis to the dermis, is composed of loose connective tissue. The papillary layer contains a large number of capillaries and neuronal axons. The capillaries nourish the epidermis and remove epidermal wastes by diffusion. The neurons provide sensory input coming from epidermal sensory receptors.
Melanoma
Melanoma is the most dangerous and lethal form of skin cancer. Melanoma tumors begin with the transformation of healthy melanocytes, which are found within the stratum basale and stratum granulosum of the epidermis, into malignant cells. This transformation is often seen when melanocytes in a normal mole become malignant. However, a melanoma tumor may begin on any portion of the skin. Because melanocytes are derived from embryonic neural crest cells, melanoma has also been known to develop within the gastrointestinal tract or brain.
Melanoma is the fifth most common cancer in men and the seventh most common cancer in women. Although the average age for the diagnosis of a melanoma tumor is 57, it is commonly found in individuals significantly younger than 55. The incidence of melanoma is increasing more rapidly world-wide than any other cancer, other than lung cancer in women.
A melanoma tumor typically spreads in width first. If left untreated the tumor then begins to grow deeper into the skin. The tumor will invade the dermis, where it develops the ability to metastasize.
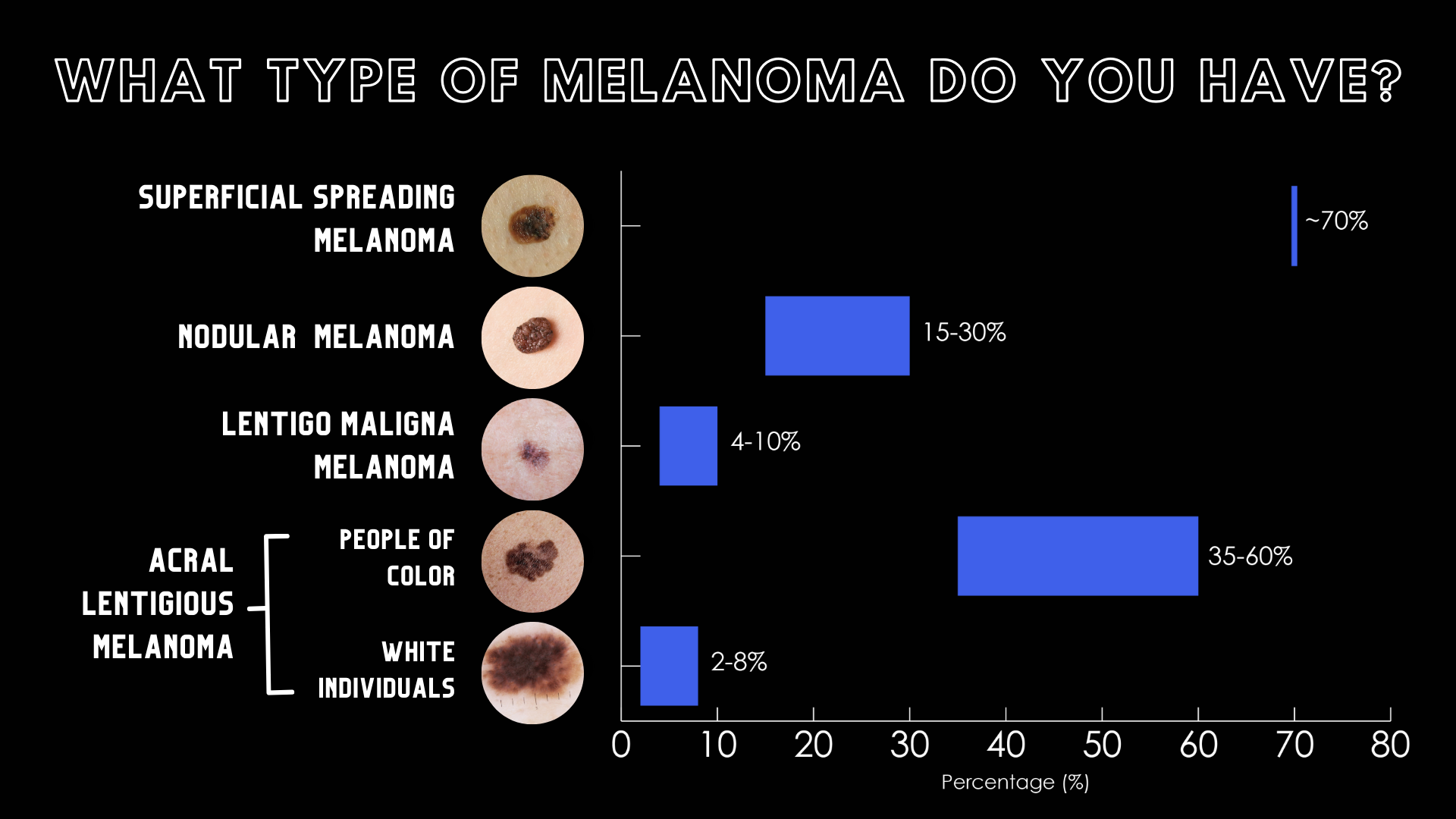
There are four different types of melanomas, which are classified according to their growth patterns.
- Superficial spreading melanoma is a tumor type which is typically flat and averages two cm. in diameter and makes up approximately seventy percent of all melanomas. The peripheral edges of the tumor may be indented, possess notches, or both. The tumor may also vary in color, or possess more than one color as you progress from the center of the tumor peripherally.
- Fifteen to thirty percent of melanoma tumors are termed nodular melanomas. These tumors are typically blue-black in color. Some, although rare, may be totally lacking in pigmentation.
- Lentigo maligna melanomas typically begin as small, freckle-like lesions. They then enlarge, becoming flat, tan lesions with a notched border. They are typically larger than three cm. in size, and account to between four and ten percent of detected melanoma lesions.
- Acral lentiginous melanomas are more common in people of color, accounting for thirty-five to sixty percent of lesions detected, as compared to two to eight percent of those detected in white individuals. These lesions, which may appear on the palms of the hands or soles of the feet, are appear as flat, brown, or tan stains with irregular borders.
The five-year survival rate for patients with stage 0 melanoma is ninety-seven percent. However, the survival rate with individuals diagnosed with a stage IV melanoma is ten percent or less.
Treatment
Surgical removal of the lesion and a significant amount of “healthy” surrounding tissue is the most common form of treatment. Associated with removal of a significant amount of surrounding tissue is also the removal and assessment of associated lymph nodes. Depending on the amount and location of the removed healthy tissue the patient may also undergo one or more skin grafts to help close the wound.
Chemotherapy treatment is often associated with the diagnosis and surgical removal of the melanoma tumor in order to help prevent the spread of malignant melanocytes via the lymphatic system.
Prevention
Self-care procedures that can help avoid melanoma or detect it in its early stages include
- Regular skin examination for rapidly growing moles or moles with unusual or irregular borders
- Avoid long-term exposure to the sun, especially between 10:00 a.m. and 2:00 p.m.
- Use of a broad-spectrum SPF thirty or higher sunscreen anytime one is out in the sun.
- Wearing protective clothing, wide-brimmed hats, and sunglasses.
- Have regular examinations by your dermatologist.
Key Terms
Stratum basale - This layer of the epidermis, which is also termed the stratum germinativum, is the deepest layer of the epidermis. This layer, which is one cell thick, possesses the highest rate of mitotic activity.
Melanocytes - These pigment-producing cells are found within the stratum basale of the epidermis. These cells possess cytoplasmic processes that inject pigment into adjacent cells within the stratum basale, as well as cells of more superficial layers. The pigment produced by melanocytes varies in color, from black to brown or yellow-brown. Differences in skin color is due to the rate of pigment synthesis, rather than the number of melanocytes present.
Nodular melanomas - Fifteen to thirty percent of melanoma tumors are termed nodular melanomas. These tumors are typically blue-black in color. Some, although rare, may be totally lacking in pigmentation.
Stratum corneum - The is the most superficial layer of the epidermis. This layer is composed of dead cells that possess a very thick cellular membrane, lack any organelles or nucleus, and possess a high amount of keratin. The intercellular connections formed within the stratum spinosum are still fully intact and bind the cells tightly together. In addition, the lipid-rich substance formed by the cells of the stratum granulosum completely surrounds the cells of this layer. These characteristics contribute to the protective nature of the stratum corneum against environmental pathogens and contribute to the cells’ water resistance.
Acral lentiginous melanomas - These melanomas are more common in people of color, accounting for thirty-five to sixty percent of lesions detected, as compared to two to eight percent of those detected in white individuals. These lesions, which may appear on the palms of the hands or soles of the feet, are appear as flat, brown, or tan stains with irregular borders.
Reticular layer - This is the deepest layer of the dermis of the skin. This layer is composed of densely interwoven connective tissue fibers that surround blood vessels, nerves, hair follicles, sweat glands, and sebaceous glands. The connective tissue fibers of this layer extend deeper into the subcutaneous tissue, and superficially into the papillary layer. As a result, all of these layers are held tightly together.
Stratum lucidum - This layer of the epidermis, which is superficial to the stratum spinosum, is found only within thick skin. Cells within this layer lack organelles and a functioning nucleus, and are densely packed together. The keratin proteins are fully formed and bind the cells of this layer tightly together.
Melanoma - The most dangerous and lethal form of skin cancer.
Integumentary system - The integumentary system, or integument, is composed of the skin and its derivatives (nails, hair, and glands).
Schedule a demo today to learn how you can incorporate BodyViz into your classes!
Schedule a Demo
Helpful Links: