Making Sense of the Corticospinal Tracts
by Robert Tallitsch, PhD | May 4, 2020
Previously in my blog about dorsal columns, I mentioned that once students understand the anatomy of the dorsal columns, the sensory information they carried, and how they were anatomically arranged, they developed a solid understanding of the other sensory tracts and their anatomical variations. The same goes for the descending motor tracts of the spinal cord. My discussion of the motor tracts always started with “general information”, and then progressed to specifics about the corticospinal system. Then I moved to the other, more complex motor tracts. My students would quickly understand the other motor tracts of the cord once they really knew and understood the anatomy of the anterior and lateral corticospinal tracts.
First the “general information” about the descending motor tracts of the CNS.
- Descending motor tracts are composed of two neurons: an upper motor neuron (UMN) and a lower motor neuron (LMN). UMN somas are located within the cerebral cortex (for the pyramidal system) or brain stem (for the extrapyramidal system), and are somatotopically arranged and are all excitatory in nature. Most UMN axons decussate to the contralateral side, either within the brain or spinal cord.
- LMN somas are located either within the brain stem or the spinal cord, and are the final pathways to the peripheral effector organs. LMNs located within the ventral horn of the spinal cord are arranged according to the medial-lateral and flexor-extensor rules.
- The medial-lateral rule states that the more medially located motor neurons innervate axial musculature, intermediate motor neurons innervate proximal limb musculature, and more laterally located neurons innervate distal limb musculature.
- According to the flexor-extensor rule LMNs innervating flexor muscles are located dorsally within the ventral horn, while LMNs innervating extensor muscles are more ventrally located.
- LMNs are either excited by the UMN or are inhibited by one or more interneurons located between the UMN and the LMN.
- The corticospinal tracts are the only direct pathway from the cerebral cortex to the LMNs in the brain stem and spinal cord. The corticospinal pathways are concerned with somatic movements, modifications of muscle tone, and segmental reflexes.
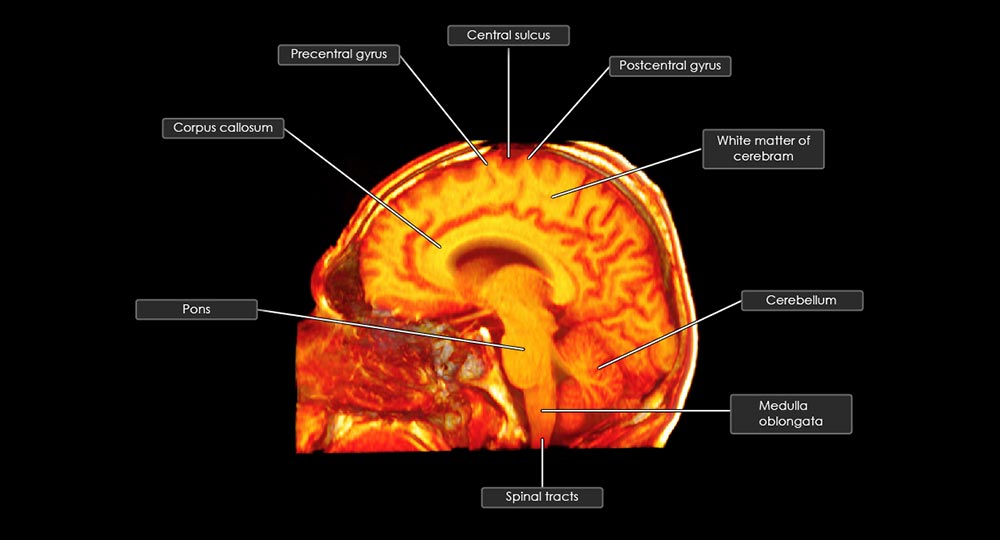
There are three corticospinal tracts: lateral corticospinal, anterior corticospinal, and corticobulbar. The first two synapse on LMNs in the ventral horn of the spinal cord. The corticobulbar synapses on motor neurons of the cranial nerves, and will not be discussed here.
80% of the UMN somas contributing to the lateral corticospinal tract (LCT) are found in the frontal lobe. Approximately 33 - 40% originate from within the premotor cortex, and 33 - 40% from the primary motor cortex. The remaining 20% originate from the somesthetic cortex of the parietal lobe. While descending within the brain the LCT gives off collateral branches to several brain structures, including basal ganglia, reticular formation, and parts of the thalamus. The LCT decussates within the medulla, and travels to the most caudal part of the cord. 55% of the tract terminates in the cervical region, 20% within the thoracic region, and 25% within the lumbosacral region. The UMNs terminate on LMNs within the ventral horn, and the LMNs of this tract follow the medial-lateral and flexor-extensor rules. As the percentages indicate, the LCT is primarily concerned with movements of the upper and lower limbs.
The UMNs of the anterior corticospinal tract (ACT) originate from the same regions of the cerebral cortex, and in the same approximate proportions as the LCT. The UMNs terminate on LMNs within the ventral horn, and the LMNs of this tract also follow the medial-lateral and flexor-extensor rules. However, the ACT has some significant differences compared to the LCT. First, the ACT carries less than 10% of the pyramidal fibers. Second, the ACT extends only to the cervical and upper thoracic regions of the cord, primarily innervating muscles of the neck, axial musculature, and proximal upper limb muscles. And, finally, ACT fibers decussate within the spinal cord just before synapsing with the LMN
A LMN lesion (lesion within the ventral horn or in the periphery) causes ipsilateral flaccid paralysis, characterized by soft, flabby, and atrophying skeletal muscles. Reflexes such as the patellar tendon reflex are absent.
UMN paralysis results from damage to a corticospinal tract anywhere along its path. The most common location for an UMN lesion is the cerebral cortex. If the lesion is superior to the site of decussation the signs and symptoms will be seen in muscles on the contralateral side. This type of damage results in skeletal muscular weakness while retaining peripheral reflex arcs. The Babinski Reflex is a diagnostic tool for an UMN lesion. Stroking the sole of the foot in a heel-to-toe direction results in the fanning of the toes accompanied by dorsiflexion of the big toe.
As I have mentioned previously, the key to really knowing anatomical information is the ability to understand and utilize anatomical facts in order to solve complex problems. Therefore, upon completion of this material, I would regularly present my students with several clinical problems dealing with various spinal tracts, which would enable me to assess whether or not they truly understood the information presented to them.
Additional Articles: