Atrial Fibrillation | BodyViz Brain Builder
by Robert Tallitsch, PhD | January 19, 2026
Case study video explaining the heart and atrial fibrillation with a patient example!
Use the button below to schedule a demo to learn about our quizzes, flash cards, and other anatomy resources that support this Brain Builder!
Schedule a Demo
According to the National Institutes of Health, atrial fibrillation is the most common cardiac arrhythmia, affecting approximately 2.5 million people in the United States. This arrhythmia, like other cardiac arrhythmias, may lead to serious complications — even death. In this Brain Builder we will discuss the anatomy of the right and left atria of the heart and the anatomy of the specialized conducting pathways in the heart. Then we will discuss the causes, symptoms, and treatment of atrial fibrillation. (For a more complete discussion of cardiac anatomy see “The Cardiovascular System and a Pacemaker.")
Internal Anatomy of the Right and Left Atria
Right Atrium
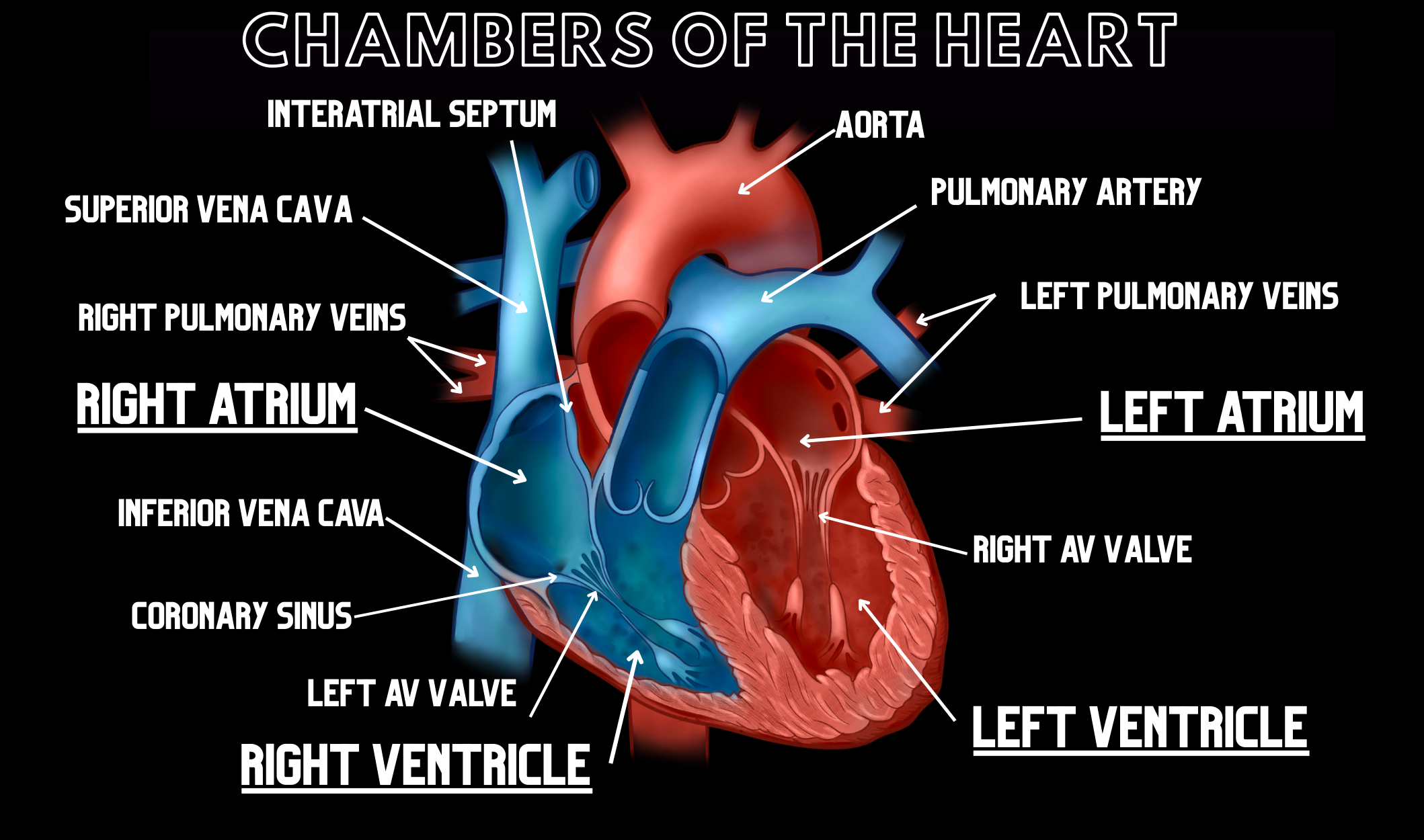
This chamber sits on the right surface of the heart. Venous blood from the periphery enters the right atrium at its upper posterior corner by the superior vena cava, and at its lower posterior corner by the inferior vena cava. Venous blood from the coronary sinus also enters the right atrium at the lower posterior corner, near the junction between the atrium and the inferior vena cava. Blood flows inferiorly into the right ventricle from the right atrium through the right atrioventricular ostium and the right atrioventricular (AV) valve.
The interior of the right atrium is divided into two parts: the posterior sinus venarum cavarum and the atrium proper. The sinus venarum cavarum, which possesses smooth walls, is formed by the openings of the superior and inferior vena cavae. The atrium proper, which includes the more anteriorly located right auricle, has rough walls due to the presence of the atrial pectinate muscles. The right auricle is an ear-like (hence the name “auricle”) muscular pouch, or appendage, that projects from the right atrium.
The interatrial septum separates the right and left atria of the heart.
Left Atrium
The left atrium forms most of the base of the heart. The left atrium receives blood from the lungs by the right and left pulmonary veins. The segment of the left atrium where the pulmonary veins enter has smooth walls. The left atrium, like the right atrium, also possesses an auricle with rough walls. However, the left atrium differs from the right atrium in that
- a greater percentage of the left atrium has smooth walls, as compared to the right atrium,
- the left auricle is significantly smaller than the right auricle, and
- the left atrium has thicker walls.
Blood flows inferiorly from the left atrium into the left ventricle through the left AV orifice. The left AV valve is found at this orifice.
Stimulating and Conducting System of the Heart
(As explained in the Brain Builder entitled “Cardiac Muscle & Cardiomyopathy") cardiac muscle differs from skeletal and smooth muscle in the following ways.
- Except for Purkinje fibers, cardiac muscle cells are considerably smaller than skeletal muscle cells.
- Unlike skeletal or smooth muscle, cardiac muscle cells branch frequently.
- Cardiac muscle cells, except for Purkinje fibers, have a single, centrally located nucleus.
- Cardiac muscle cells possess specialized cell junctions called intercalated discs. These structures allow the spread of an action potential from cardiac muscle cell to cardiac muscle cell, thereby forming a functional syncytium.
In a normally functioning heart, the atria and ventricles contract in a way that allows them to function together as one pump. This is accomplished by the stimulating and conducting system of the heart. These specialized cardiac muscle cells produce and move action potentials throughout the heart in such a way as to produce a synchronous and effective pumping system.
The stimulating and conducting system of the heart is composed of the Sinoatrial (SA) node, the Atrioventricular (AV) node, the AV bundle, right and left bundle branches, and the subendocardial branches.
Sinoatrial (SA) node
The SA node is located just deep to the epicardium at the junction of the superior vena cava and the right atrium. The SA node is a small collection of specialized cardiac muscle cells that have the ability to spontaneously depolarize, thereby generating an action potential. As such, the SA node serves as the pacemaker of the heart. In this role the SA node initiates these electrical impulses approximately seventy times per minute. These impulses then spread throughout the heart and generate the rhythmic contractions of the entire heart.
The electrical impulses generated by the SA node travel through both atria, causing them to contract, aiding in the flow of blood from the atria into the ventricles. In addition, these impulses also travel through the wall of the right atrium to the AV node by myogenic conduction (conduction through muscle cells).
Atrioventricular (AV) node
The AV node is a smaller aggregation of cells than the SA node. It is located in the interatrial septum near the opening of the coronary sinus. The AV node passes the electrical signal to the ventricles through the AV bundle.
AV Bundle
The AV bundle is the only group of myocardial cells that pass from the atria to the ventricles of the heart. It does so by passing through the fibrous skeleton of the heart along the membranous portion of the interventricular septum.
Right and Left Bundle Branches and the Subendocardial Branches
The AV bundle divides into the right and left bundle branches in the interventricular septum. The branches proceed on each side of the interventricular septum into the right and left ventricles as subendocardial branches. These subendocardial branches are composed of Purkinje fibers, which pass into the myocardium of the right and left ventricles.
Impulse generation and transmission through the heart by the stimulating and conducting system of the heart is summarized as follows:
- The SA node spontaneously depolarizes and initiates an action potential. This action potential travels rapidly through both atria, causing the atria to contract.
- This action potential travels from the SA node to the AV node by myogenic conduction.
- The action potential passes through the AV node into the AV Bundle. From the AV bundle the signal passes into the right and left bundle branches, which conduct the signal into the subendocardial branches of both ventricles. This initiates ventricular contraction.
Atrial Fibrillation
Atrial fibrillation (also termed AFib) is a very rapid, irregular, and uncoordinated heart rhythm that typically starts within the right atrium. It may, however, start within either atrium. During AFib the atrial contractions are out of synch with the ventricular contractions. This interferes with ventricular filling and, therefore, reduces the amount of blood pumped out by the ventricles.
Causes of Atrial Fibrillation
Some form of cardiac pathology is often the cause of AFib. However, other pathologies have been known to contribute to the development of atrial fibrillation. Some causes that may contribute to the development of atrial fibrillation include.
Various cardiac pathologies, including
- A congenital cardiac abnormality
- Heart valve abnormality
- A previous heart attack
- An abnormality within the SA node (sometimes referred to as “sick sinus syndrome”)
- Coronary artery disease
- Other causes that may contribute to AFib
- Kidney disorder resulting in altered blood electrolyte levels
- Pneumonia
- High blood pressure
- Hyperactive thyroid gland
- Sleep disorder, such as sleep apnea
- Excess consumption of alcohol or caffeine
- Smoking
- OTC medications containing stimulants, such as cold or allergy medications
- Obesity
Types of Atrial Fibrillation
Although one may refer to the “types” of atrial fibrillation, today’s medical literature classifies AFib by its duration. These classifications are:
- Persistent Atrial Fibrillation: AFib lasting for a week or longer. Persistent atrial fibrillation lasting for a year or more is termed Long-Standing Persistent Atrial Fibrillation.
- Paroxysmal Atrial Fibrillation: AFib lasting less than a week. This type of AFib may stop on its own only to restart at a later date. Paroxysmal AFib can, and often does progress into persistent atrial fibrillation.
- Valvular Atrial Fibrillation: This type of atrial fibrillation may be initiated by a problem with an artificial valve or one or more of the natural valves within the heart.
- Nonvalvular Atrial Fibrillation: In this type of AFib the cause is something other than a defective heart valve. The underlying problem typically occurs in an older individual that has chronically had one or more of the pathologies or characteristics listed above.
Symptoms, Diagnosis, and Consequences of Atrial Fibrillation
The most common symptom of AFib is fatigue or extreme and chronic tiredness. Other symptoms may include
- heart palpitations, or the feeling that your heart is beating too fast or skipping a beat,
- difficulty breathing,
- mild to severe chest pain,
- dizziness or fainting.
One of the most common ways to diagnosis AFib is for the patient to wear a Holter monitor. A Holter monitor is a portable ECG (electrocardiogram) recorder. Typically the physician will require the patient to wear the monitor for a prolonged period of time (several days to a week or more) in order to determine if the patient has AFib and how long it persists.
The most serious medical concern for a patient with AFib is the development of blood clots, which might result in a stroke. Because of the uncoordinated atrial contractions during AFib the atria are unable to pump out all of the blood into the ventricles. As a result, blood begins to pool within the atria and auricles. The pooling of blood increases the possibility of the formation of numerous blood clots of various sizes. These clots may remain within the heart or may travel to another location within the body. If one or more of these clots is pumped out of the heart and travels to the brain the chances of an embolic stroke within the brain increases significantly.
Treatment of Atrial Fibrillation
AFib is typically treated by one or more of the following procedures: medication, nonsurgical treatment, or minimally invasive surgical treatment.
Medication and nonsurgical Treatments:
An abnormal heartbeat like atrial fibrillation is difficult to treat with medications. As a result, most patients with AFib will be prescribed medications intended to lessen the chances of developing blood clots.
Nonsurgical treatments for AFib typically involve one or more forms of cardioversion — the administration of an electrical shock in an effort to “reset” the cardiac rhythm and stop the atrial fibrillation. External cardioversion involves the external administration of an electrical shock on the outside of the chest in an effort to stop the atrial fibrillation.
Minimally Invasive Surgical Treatments:
If external cardioversion does not eliminate the fibrillation the physician may opt for a procedure termed catheter ablation. In this procedure a catheter is inserted into a vein and guided to the heart. Utilizing a small electrode the physician destroys the cardiac tissue that is thought to be the cause of the atrial fibrillation.
One new form of minimally invasive surgical treatment for atrial fibrillation involves the implantation of a newly developed device termed the WatchmanTM.
The use of blood thinners puts a patient at risk for severe external or internal bleeding. In addition, the success rate of cardioversion is quite variable and may not be permanent. As a result, the medical profession has sought other forms of treatment for nonvalvular atrial fibrillation. One of the newest minimally invasive surgical treatments for clot prevention associated with nonvalvular atrial fibrillation is the implantation of a device termed the WatchmanTM.
The WatchmanTM is a small device shaped like a parachute. The device is implanted by inserting a catheter into the femoral vein. The catheter is then guided into the left auricle of the patient’s heart. Once the WatchmanTM is in place the catheter is removed and the incision is closed by several small sutures. The patient will be monitored in the hospital for 24 to 48 hours to ensure that the WatchmanTM remains in place. Following discharge the patient will continue taking blood thinners for up to six weeks following implantation of the WatchmanTM, after which the use of blood thinners may be discontinued permanently.
Long term prognosis:
A patient with atrial fibrillation is at risk of developing blood clots that might result in a stroke. Treatment, be it with blood thinners, cardioversion, minor or major surgery is frequently successful in the prevention of blood clot formation. With such treatment the patient is able to live a healthy life with minimal complications.
Schedule a demo today to learn how you can incorporate BodyViz into your classes and give your students the opportunity to practice using the information from this Brain Builder on real patients with authentic 3D dissection!
Schedule a Demo
Helpful Links: